Cystinosis
What is cystinosis?
Cystinosis is a genetic condition that most frequently impacts the eyes and kidneys. It causes the amino acid cystine to build up in the body’s cells, damaging them. Crystals can then form that cause damage to organs and tissues.
While the condition is rare, it is dangerous and causes long-term damage to the body. Many individuals with cystinosis end up in kidney failure.
What causes cystinosis?
Cystinosis is a genetic condition. This means that it is caused by an abnormality in the person’s DNA. Cystinosis has no correlation to a particular sex or ethnicity.
Genetics and genetic conditions
DNA, which is present in every cell of the body, carries instructions for how the body is built. Genes are segments of DNA that contain the information for different physical traits (such as eye color). Genes are passed from parent to child. This means a child will have two copies of each gene, one from each parent. Each copy of a gene is called an allele. Alleles will determine how a trait is expressed (such as blue or brown eye color).
These inherited alleles will be either dominant or recessive. A dominant allele is one that will override the other allele. Say a child inherits one dominant allele for brown eyes and one recessive allele for blue eyes. The dominant allele will take over, and the child will develop brown eyes.
Recessive alleles will only express themselves if there are two of them. This means the child will need the recessive allele for blue eyes from both parents in order to develop blue eyes.
An important thing to note is that many physical traits are built up of multiple genes. This means that a trait like eye color will rely on more than just one gene.
If one parent has a recessive mutation on one of their alleles, they are called a carrier. Because the allele is recessive, the parent won’t experience symptoms of the mutation. The other allele is normal and so compensates for the allele with the mutation.
However, if both parents are carriers, there is a 1-in-4 (25%) chance that one of their children will inherit both recessive alleles. If the child does, they will experience the effects of the genetic mutation. There is also a 2-in-3 (66%) chance that other children of these parents will be carriers of the allele with the genetic mutation.
Genetic conditions are what develop when an individual has these mutated alleles. These mutations mean that the allele carries instructions that end up causing a defect of the body. It might be missing a part or have too many parts, or it just might be the wrong shape. While it is possible for the mutations to occur in different parts of our body after we are born, they are usually passed from parent to child.
The genetics of cystinosis
Cystinosis is caused by a genetic mutation of a gene called CTNS. This gene tells the body how to make the transporter protein cystinosin.
Cystine is made up of two cysteine amino acids that are bonded together. Cystinosin is in charge of transporting cystine in our cells. Cystine is an important part of the body’s ability to make collagen. This means it impacts skin’s elasticity. Cystine is present in many other parts of our body, where it is essential in helping enzymes function correctly.
The mutation of CTNS prevents cystinosin from properly transporting cystine. This causes cystine to build up and form into crystals that damage cells throughout the body.
What are the types of cystinosis?
There are three forms of cystinosis. All three types are caused by the same genetic mutation. However, they vary in the age symptoms begin as well as in the severity of symptoms.
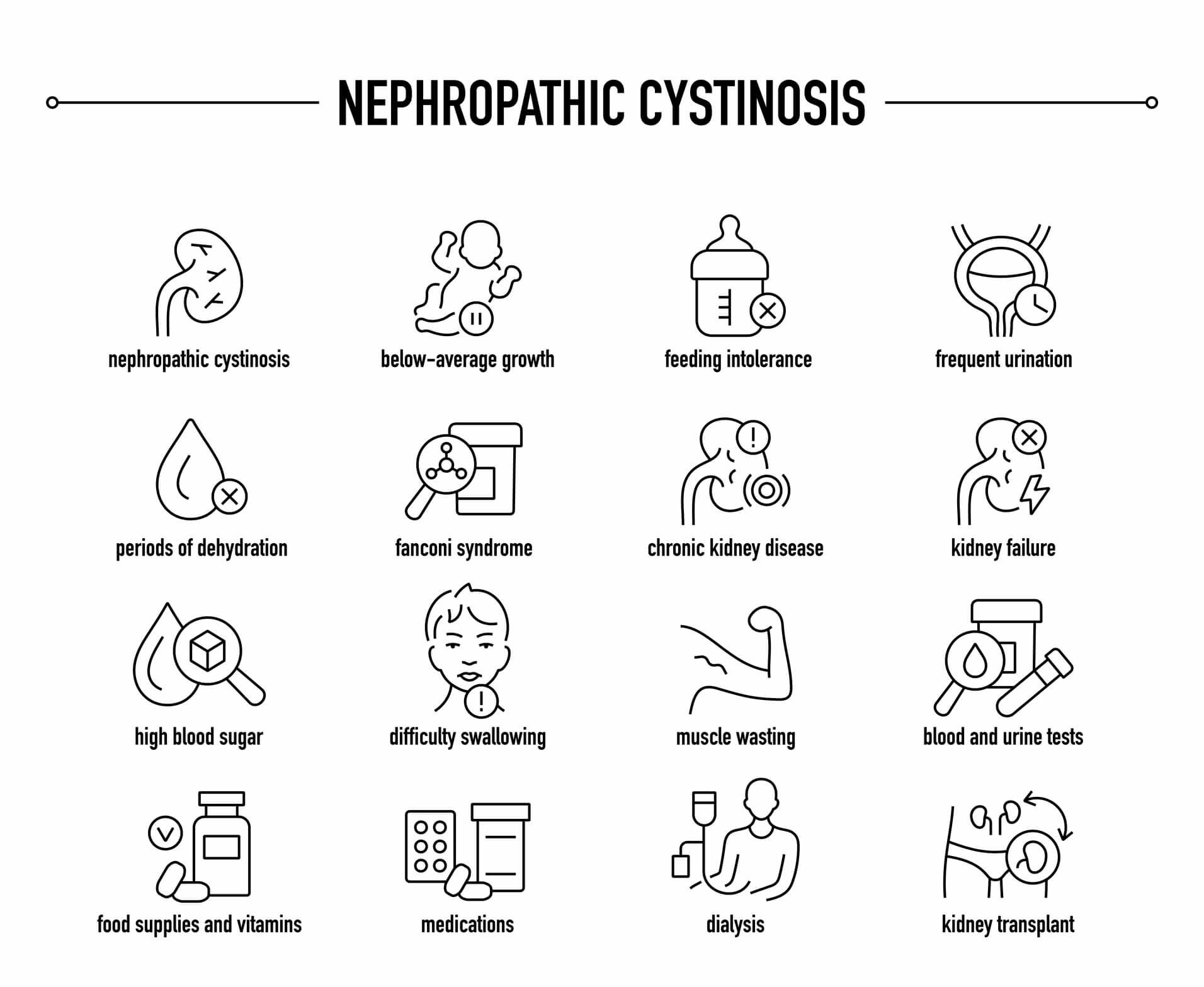
Nephropathic cystinosis
Nephropathic cystinosis is the most common form. It accounts for 95% of cystinosis cases. Those with this form will usually begin to show symptoms at around 1 year old. However, the cystine will have started building up before birth. If not properly treated, those with nephropathic cystinosis are at high risk of end-stage renal failure by the time they are 10.
Juvenile nephropathic cystinosis
Juvenile nephropathic cystinosis appears slightly later, typically between ages 10 and 20. While its symptoms are often the same as nephropathic cystinosis, they will be less severe. However, there is still a high risk of renal failure. These individuals sometimes receive diagnosis because of vision changes like photophobia (light sensitivity).
Non-nephropathic cystinosis
Non-nephropathic cystinosis is unique in that the buildup of cystine is only in the eyes. Because it is milder, it can sometimes go undiagnosed until the individual is an adult. These individuals rarely have the renal issues that characterize the nephropathic forms. However, it is still important for those with non-nephropathic cystinosis to monitor their renal health.
What are the symptoms of cystinosis?
The earliest signs of nephropathic cystinosis often center around the kidneys. The affected child may have both excessive thirst and excessive urination. They often show a failure to thrive, which is characterized by very slow physical growth.
The child may also develop rickets, which causes the bones to be soft and can result in bone deformities. Other symptoms include vomiting, fever, photophobia and difficulty swallowing.
Many of these symptoms can be tied to the development of Fanconi syndrome. Fanconi syndrome is a defect in a part of the kidneys known as the proximal tubule.
The proximal tubule is in charge of absorbing certain necessary nutrients. Fanconi syndrome prevents the proximal tubule from absorbing these substances. This can lead to nutritional deficiencies and dehydration.
In juvenile nephropathic cystinosis, these same signs and symptoms are often present. The adolescent may also show signs of muscle weakness, fatigue and delayed puberty.
Vision changes can occur in any of the three versions of cystinosis. However, non-nephropathic cystinosis is unique. It is the only version in which ocular issues are the main (and often only) symptoms. For these individuals, cystine crystals build up in the cornea.
The cornea is the clear layer over the very front of the eye. Its dome shape helps focus light as it enters the eye. These crystals are very small and needle shaped and are evenly distributed in the cornea. This cystine buildup can lead to corneal opacity or cloudiness. In most cases, photophobia (sensitivity to light) is the only sign of cystinosis.
READ MORE about other conditions that affect the cornea
Cystine crystals can build up in other parts of the eye as well. This may happen in the conjunctiva, iris, lens and retina. Very few other health conditions present with both photophobia and corneal crystals. These include multiple myeloma and Bietti crystalline corneal dystrophy.
How is cystinosis diagnosed?
A physician can diagnose cystinosis by measuring the amount of cystine in the patient’s white blood cells. They may also check the patient’s urine for loss of potential nutrients, as this can indicate Fanconi syndrome.
An eye doctor can also use a slit-lamp to examine the patient’s corneas for cystine crystals. A slit-lamp is a microscope with a bright light attached to it. It allows the eye doctor to more closely examine the front and inside of the eye.
Another diagnostic avenue is genetic testing. It allows the physician to specifically look for a mutation of the CTNS gene. Prenatal testing is also available for families who are known carriers of the mutation. Testing will determine if their baby will be born with the condition.
How is cystinosis treated?
The most common initial treatment for cystinosis is cysteamine. This is a medication that reduces the body’s levels of cystine. It can help slow down the progression of kidney damage. For those with cystine crystals in their corneas, there are also cysteamine eye drops. These drops help dissolve the crystals and reduce light sensitivity.
Treatments for children who have developed Fanconi syndrome focus on replenishing lost nutrients. These treatments include:
Extra fluid intake to prevent dehydration.
Medications to help with electrolyte balance.
Medications that help the kidneys absorb phosphate.
Even with treatment, individuals who have cystinosis still often develop end-stage renal disease. Many with nephropathic and juvenile nephropathic cystinosis will eventually need kidney transplants. This can also cure Falconi syndrome. However, cystine will continue to build up in other areas of the body.
What is the prognosis with cystinosis?
Cystinosis used to be fatal. However, the life expectancy of someone with cystinosis is now much longer if they are treated. Early diagnosis means that steps can be taken to slow the progression of the condition. Lifelong use of cysteamine can also help prevent complications.
Those with nephropathic cystinosis are at high risk of developing kidney failure. This means they will likely require dialysis and an eventual kidney transplant.
When should you see a doctor?
Seek medical help if your child is showing signs of dehydration, excessive urination and excessive thirst. If you or your child begin experiencing sudden sensitivity to light, check in with your eye doctor. Maintaining yearly eye exams is also important. Regular exams allow eye doctors to track any potential buildup of cystine crystals in the cornea and other eye structures.
Cystinosis. Cleveland Clinic. January 2023.
DNA, genes & chromosomes. Cleveland Clinic. May 2022.
Is eye color determined by genetics?. MedlinePlus [Internet]. July 2022.
Genes and genetics explained. Better Health Channel. Department of Health, State Government of Victoria, Australia. September 2019.
Cystinosis 101. Cystinosis Research Network. Accessed July 2023.
Cysteine. Health Encyclopedia. University of Rochester Medical Center. Accessed July 2023.
Cystine. Health Encyclopedia. University of Rochester Medical Center. Accessed July 2023.
Nephropathic cystinosis: Symptoms, treatment, and perspectives of a systemic disease. Frontiers in Pediatrics. March 2018.
Cystinosis. Genetic and Rare Diseases Information Center. February 2023.
Fanconi syndrome. StatPearls [Internet]. July 2023.
Cystinosis. National Organization for Rare Disorders. August 2022.
Latest clinical approaches in the ocular management of cystinosis: A review of current practice and opinion from the ophthalmology cystinosis forum. Ophthalmology and Therapy. September 2018.
What is a slit lamp?. EyeSmart. American Academy of Ophthalmology. April 2018.
Page published on Wednesday, September 27, 2023
Page updated on Tuesday, October 3, 2023
Medically reviewed on Tuesday, August 1, 2023






